Imagine this: you’re at the grocery store, browsing the aisles, when a crushing chest pain stops you in your tracks. You’re sweating, breathless, and fear grips your heart. This is not a scene from a movie; it’s the reality of acute coronary syndrome (ACS), a serious heart condition that can strike seemingly out of nowhere. As a nurse, understanding the warning signs and implementing appropriate diagnoses for ACS is crucial for saving lives. This article delves into the intricacies of nursing diagnoses for ACS, unraveling the critical role nurses play in managing this complex condition.
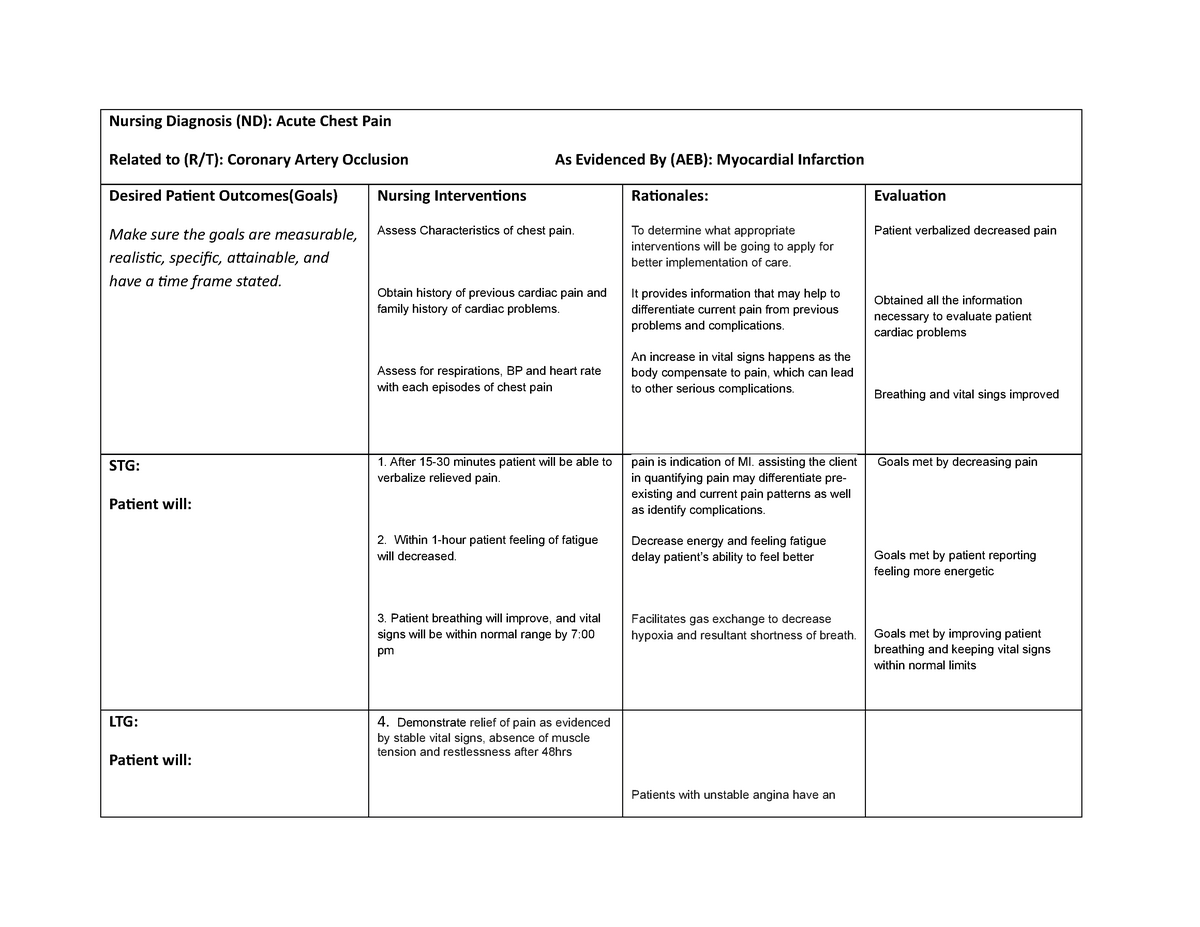
Image: www.pelajaran.guru
Acute coronary syndrome is a broad term encompassing a range of conditions where the blood supply to the heart is suddenly and severely reduced. The most common forms of ACS are unstable angina, which causes chest pain but no permanent heart damage, and myocardial infarction (MI), commonly known as a heart attack, in which heart muscle dies due to lack of blood flow.
Unveiling the Heart’s Silent Cry: Recognizing ACS
Nurses are often the first point of contact for patients experiencing symptoms of ACS. Their ability to recognize the warning signs and assess the patient’s needs is critical for swift and effective intervention. This begins with a thorough understanding of the potential symptoms.
Detecting the Hallmarks of ACS
The typical “elephant on the chest” pain is often the most prominent sign, described as a crushing, squeezing sensation that may radiate to the arms, neck, or jaw. However, it’s important to remember that individuals may experience ACS in a multitude of ways. Some symptoms may be more subtle, including:
- Unusually intense fatigue: This may be a sign that the heart can’t pump blood efficiently due to the blockage in the arteries.
- Chest tightness, burning, or pressure: A feeling of “heaviness” in the chest can be a hallmark of ACS.
- Shortness of breath: A sudden difficulty breathing, especially when exertion is involved, could be a sign of a heart attack.
- Nausea and vomiting: ACS can trigger stomach upset in some individuals.
- Pain in the jaw, neck, or back: The pain can also radiate to the shoulders, arms, or jaw.
- Sudden sweating: This may be a sign of the body’s stress response to the lack of blood flow to the heart.
Nursing Assessments: Gathering Vital Information
Once a patient presents with potential ACS, nurses conduct thorough assessments to gather vital information, including:
- Medical History: A complete medical history, focusing on prior heart conditions, diabetes, high blood pressure, and family history of heart disease, helps nurses understand the patient’s risk factors and establish a baseline.
- Physical Examination: Vital signs such as heart rate, blood pressure, respiration, and temperature provide crucial clues about the patient’s overall health status.
- Electrocardiogram (ECG): A vital tool, ECG measures the electrical activity of the heart, providing a detailed picture of the heart’s rhythm and revealing signs of ischemia (reduced blood flow) or a heart attack.
- Blood Tests: Lab tests, including troponin levels, which indicate heart muscle damage, are crucial for confirming a diagnosis and guiding treatment.

Image: www.pinterest.com
Navigating the Labyrinth of Nursing Diagnoses for ACS
Once the necessary assessments are completed, nurses can begin formulating nursing diagnoses, which provide a framework for planning individualized patient care. Several nursing diagnoses are relevant to ACS, each focusing on a specific aspect of the patient’s condition and care needs.
Key Nursing Diagnoses for ACS
- Ineffective Tissue Perfusion (Cardiac): This diagnosis emphasizes the reduced blood flow to the heart muscle, which is the core issue in ACS.
- Acute Pain: The severe crushing chest pain experienced by many individuals experiencing ACS is a significant concern, requiring targeted pain management strategies.
- Anxiety: The fear and uncertainty associated with acute illness, coupled with the potential seriousness of ACS, can lead to heightened anxiety.
- Impaired Gas Exchange: ACS can impact the heart’s ability to pump blood effectively, leading to oxygen deprivation and impaired gas exchange.
- Activity Intolerance: Patients with ACS may experience weakness and fatigue, limiting their ability to participate in daily activities.
- Risk for Decreased Cardiac Output: This diagnosis addresses the potential for the heart’s ability to pump blood effectively to be compromised due to the impact of ACS.
The Art of Care: Managing ACS With Compassion and Skill
The nursing care of individuals experiencing ACS is a multifaceted process that necessitates a high degree of skill, knowledge, and compassion. Nurses play a critical role in monitoring the patient’s status, administering medications, providing emotional support, and educating the patient and family about the condition and its management.
Pain Management: Easing the Heart’s Anguish
One of the most important aspects of nursing care for ACS is pain management. Nurses administer medications, including nitrates and opioids, to alleviate chest pain. They also provide comfort measures, such as positioning the patient for optimal comfort and offering calming therapies.
Monitoring and Support: The Heartbeat of Care
Nurses meticulously monitor the patient’s vital signs, ECG, and lab results, carefully assessing for signs of deterioration or improvement. Their constant vigilance allows for prompt interventions to maintain stability. They also provide emotional support, explaining the procedures and treatments, and addressing the patient’s fears and concerns.
Education and Empowering Patients: Taking Charge of Heart Health
Nurses are instrumental in educating patients and their families about ACS, its causes, risk factors, and long-term management. They empower patients to take an active role in their health by providing them with information about lifestyle changes, medication adherence, and follow-up care.
The Path Forward: Navigating Recovery and Preventing Future Events
ACS is not merely a crisis; it’s a significant life event that prompts a change in lifestyle and a renewed focus on heart health. Nurses provide guidance and support throughout the recovery process, working collaboratively with the patient and other healthcare professionals to develop an individualized care plan.
Rehabilitation and Lifestyle Modifications: Rebuilding Strength
Cardiac rehabilitation programs are vital after ACS, helping patients regain strength, improve cardiovascular fitness, and manage risk factors. Nurses play a key role in educating patients about cardiac rehabilitation programs, encouraging their participation, and supporting their progress.
Medication Management: A Shield Against Future Heart Trouble
Nurses reinforce the importance of medication adherence, explaining how each medication works and its significance in preventing future heart events. They also educate patients about potential side effects and encourage them to report any unexpected reactions.
Nursing Diagnosis For Acute Coronary Syndrome
The Nurse’s Role: A Steadfast Guardian of Heart Health
Nurses are the heart of the healthcare team, providing unwavering care and support to individuals experiencing ACS. They are not only skilled clinicians but also compassionate caregivers, understanding the emotional, physical, and psychological impact of this life-changing event. Their expertise in recognizing symptoms, accurately diagnosing, and initiating appropriate medical interventions can make the difference between life and death.
Through their knowledge, skills, and unwavering dedication, nurses empower patients to take charge of their heart health, fostering resilience and improving their chances of a longer, healthier life.
Call to Action:
Have you experienced or witnessed someone experiencing symptoms of ACS? Share your experiences in the comments below and let’s learn from one another. By understanding this condition, we can all become champions of heart health, protecting ourselves and those we love.






