Imagine a patient struggling to breathe, their lungs congested, their ankles swollen, and their heart racing. This is the reality of fluid volume excess, a condition where the body retains too much fluid, leading to various health complications. As a nurse, I have witnessed firsthand the challenges this condition poses to patients and the vital role nursing care plays in managing fluid overload.

Image: simplenursing.com
Fluid volume excess, also known as hypervolemia, can be caused by a myriad of factors, from heart failure and kidney disease to excessive intravenous fluid administration. It’s a condition that requires careful assessment, monitoring, and a comprehensive nursing care plan to ensure the patient’s safety and well-being. This article will delve into the intricacies of fluid volume excess and provide an in-depth guide to developing effective nursing care plans.
Understanding Fluid Volume Excess
What is Fluid Volume Excess?
Fluid volume excess occurs when there is an imbalance between fluid intake and output, resulting in an excessive buildup of fluid in the body’s circulatory system. While our bodies naturally regulate fluid levels, certain medical conditions or external factors can disrupt this delicate balance.
Causes of Fluid Volume Excess
The causes of fluid volume excess are diverse, encompassing various medical conditions and external influences. Some common causes include:
- Heart failure: A weakened heart cannot effectively pump blood, leading to fluid buildup in the lungs and extremities.
- Kidney disease: Impaired kidneys fail to filter waste products and excess fluid, resulting in fluid retention.
- Liver disease: The liver’s inability to produce albumin, a protein essential for maintaining fluid balance, contributes to fluid overload.
- Excessive intravenous (IV) fluid administration: Overzealous IV fluid replacement can lead to fluid overload.
- Premenstrual syndrome (PMS): Fluid retention is a common symptom of PMS due to hormonal fluctuations.
- Medications: Certain medications, such as corticosteroids and nonsteroidal anti-inflammatory drugs (NSAIDs), can cause fluid retention.
- High sodium intake: Consuming excessive salt can lead to fluid retention through osmosis.
- Congestive heart failure (CHF): The heart is not able to pump blood effectively, causing fluid to back up in the lungs, legs, and feet.
- Coronary artery disease (CAD): This condition can lead to heart failure, which in turn can cause fluid volume excess.
- Peripheral vascular disease (PVD): This condition can affect blood flow to the legs and feet, causing fluid buildup.
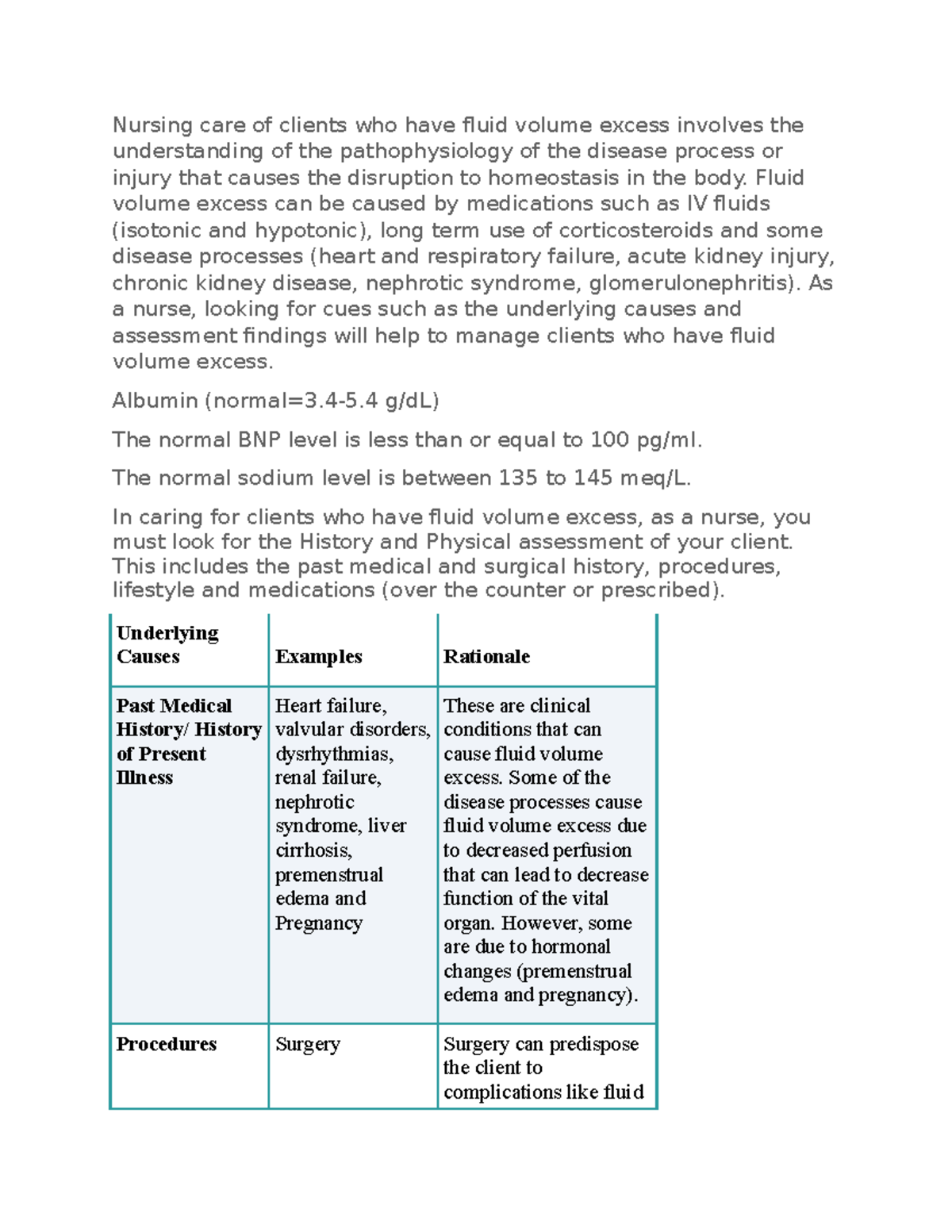
Image: www.studocu.com
Symptoms of Fluid Volume Excess
Recognizing the symptoms of fluid volume excess is crucial for timely intervention and preventing complications. Common symptoms include:
- Edema: Swelling in the ankles, feet, legs, hands, and face.
- Dyspnea: Difficulty breathing, shortness of breath, especially when lying down.
- Rapid weight gain: Sudden weight gain, often more than 2 pounds in a day, is a significant indicator.
- Increased blood pressure: Elevated blood pressure due to increased blood volume.
- Tachycardia: Rapid heartbeat, as the heart tries to compensate for increased fluid volume.
- Distended neck veins: Visible bulging veins in the neck due to increased pressure in the circulatory system.
- Crackles in the lungs: Abnormal sounds heard during auscultation, indicating fluid buildup in the lungs.
- Increased urine output: Initially, the body may try to compensate by excreting excess fluid, leading to increased urination.
- Fatigue: A feeling of tiredness and weakness due to the heart working harder to pump the increased blood volume.
- Headache: Fluid overload can increase pressure in the brain, causing headaches.
Fluid Volume Excess Nursing Care Plan: Implementing Interventions
Once fluid volume excess is identified, a comprehensive nursing care plan must be implemented to manage the condition and alleviate the patient’s symptoms. Here are some key nursing interventions:
1. Assessment and Monitoring
The first step is to conduct a thorough assessment of the patient’s symptoms and medical history. Vital signs, including blood pressure, heart rate, respiratory rate, and temperature, need to be closely monitored for signs of deterioration. Regularly assess for edema and monitor daily weight changes to track fluid balance.
2. Fluid Restriction
Depending on the severity of the fluid overload, a fluid restriction may be necessary. Collaborate with the healthcare provider to establish appropriate fluid intake limits and ensure the patient understands and adheres to the restrictions.
3. Medication Administration
Medications can play a significant role in managing fluid volume excess. Diuretics, such as furosemide (Lasix) and hydrochlorothiazide (HydroDIURIL), help eliminate excess fluid by increasing urine production. Other medications might include vasodilators, which help relax blood vessels and reduce blood pressure, and medications to treat the underlying cause of fluid overload.
4. Positioning
Proper positioning can improve respiratory function and reduce pressure on the lungs. Elevate the patient’s head of bed to 30 degrees or higher to reduce pulmonary congestion. Encourage deep breathing exercises and use an incentive spirometer to promote lung expansion.
5. Oxygen Therapy
Patients experiencing dyspnea may require supplemental oxygen therapy. Monitor oxygen saturation levels and adjust the oxygen flow rate as needed. Ensure the patient receives adequate oxygenation.
6. Diet Modifications
Dietary interventions can help manage fluid overload. Encourage a low-sodium diet to prevent fluid retention. Offer patients fluids sparingly and monitor their intake carefully. Limit caffeine and alcohol, which can contribute to fluid retention.
7. Leg Elevation
Elevate the patient’s legs above the heart for several hours each day. This maneuver encourages drainage of fluid from the legs and reduces edema.
8. Antiembolism Stockings
Encourage the use of antiembolism stockings to improve circulation and prevent deep vein thrombosis, a potential complication of fluid overload.
Tips and Expert Advice for Managing Fluid Volume Excess
Here are some tips and expert advice to improve your nursing care for patients with fluid volume excess:
1. Prioritize Patient Education
Educate patients about the importance of following their prescribed fluid restrictions, medication regimen, and dietary modifications. Explain the potential complications of fluid overload and emphasize the importance of regular follow-ups with their healthcare providers.
2. Promote Patient Independence
Empower patients to actively participate in their care. Encourage them to track their daily weight, monitor their fluid intake, and report any unusual symptoms to their healthcare providers. This fosters a sense of control and ownership over their health.
3. Collaborate with the Healthcare Team
Maintain open communication with physicians, pharmacists, and other members of the healthcare team to ensure continuity of care. Discuss any concerns or changes in the patient’s condition to optimize their treatment plan.
4. Advocate for your Patients
Advocate for your patients’ needs and ensure they receive appropriate care. When necessary, escalate concerns to the healthcare provider to prevent complications. By advocating for your patients, you can help improve their outcomes and enhance their quality of life.
Frequently Asked Questions (FAQs)
- What are the potential complications of fluid volume excess?
- How long does it take for fluid volume excess to resolve?
- Are there any lifestyle changes that can help prevent fluid volume excess?
- Can I use home remedies to alleviate fluid retention?
- Does fluid volume excess affect different individuals differently?
Uncontrolled fluid overload can lead to serious complications, including pulmonary edema (fluid buildup in the lungs), heart failure, and even death. Early intervention and effective management are critical to prevent these complications.
The duration of fluid overload varies depending on the underlying cause and severity. Some conditions, such as premenstrual fluid retention, may resolve within a few days. Others, like heart failure, may require long-term management.
Yes, following a healthy lifestyle can help prevent fluid overload. Maintaining a balanced diet low in sodium, staying hydrated, getting regular exercise, and managing underlying medical conditions are crucial.
It’s important to consult with your healthcare provider before trying any home remedies. Some natural remedies, such as dandelion tea and ginger, may have diuretic properties. However, they should not be used as a substitute for medical advice. Please consult with a qualified healthcare professional.
Yes, the severity of fluid overload and its impact on individuals can vary. Factors that influence the effects include age, underlying health conditions, and the cause of fluid retention.
Fluid Volume Excess Nursing Care Plan
https://youtube.com/watch?v=93A1NDTc5ng
Conclusion
Fluid volume excess is a complex condition that requires a comprehensive nursing care plan to ensure the best possible outcomes for patients. By implementing effective interventions such as assessment, monitoring, fluid restriction, medication administration, and positional changes, nurses play a vital role in managing fluid overload and preventing complications. Remember, empowering patients through education, promoting independence, collaborating with the healthcare team, and advocating for their needs are essential components of quality nursing care. By embracing these principles, nurses can make a significant difference in the lives of patients with fluid volume excess.
Are you interested in learning more about fluid volume excess or other nursing care topics? Let me know your thoughts in the comments below!






